
Blog
-
Athlete's Foot: Recognizing and Treating Fungal Infections
posted: May 01, 2024.

-
Diabetic Foot Care: Importance, Tips, and Warning Signs
posted: Apr. 08, 2024.

-
Symptoms of an Ingrown Toenail
posted: Apr. 01, 2024.

-
Find Relief From Your Heel Pain
posted: Mar. 27, 2024.

-
Treating Plantar Fasciitis
posted: Mar. 16, 2024.

-
Complications of Untreated Hammertoes
posted: Mar. 14, 2024.

-
Managing Your Heel Pain
posted: Mar. 01, 2024.

-
The Role of Podiatry in Managing Foot and Ankle Fractures
posted: Feb. 09, 2024.

-
What You Need To Know About Ingrown Toenails
posted: Feb. 01, 2024.

-
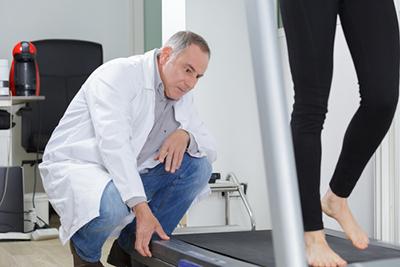
Sports Podiatry: Addressing Foot and Ankle Injuries in Athletes
posted: Jan. 08, 2024.

-
Orthotics and Their Role in Foot Health: Custom Solutions for Various Conditions
posted: Jan. 01, 2024.

-
Diabetic Foot Care: Preventing Complications and Maintaining Foot Health
posted: Dec. 07, 2023.

-
Preventing Foot Injuries: Tips for Proper Foot Care and Injury Avoidance
posted: Dec. 01, 2023.

-
The Benefits of Seeing a Podiatrist
posted: Nov. 07, 2023.
-
The Benefits Of Orthotics
posted: Nov. 01, 2023.

-
When To See a Podiatrist
posted: Oct. 06, 2023.

Contact Us
Please enter the following:
Our Location
North West
5471 Georgetown Road Suite C Indianapolis
Plainfield
2230 Stafford Rd. Suite 145 Plainfield
South
8615 US 31 Suite A Greenwood
East
9670 East Washington Suite 215 Indianapolis
Downtown
1801 Senate Blvd. Suite 610 Methodist IU Campus
Carmel
12425 Old Meridian St. Ste A-2 Carmel
North East7950 N Shadeland Ave Suite 100 Indianapolis
7950 N Shadeland Ave Suite 100 Indianapolis
Fishers/Saxony13436 Tegler DriveSuite 100 Noblesville
13436 Tegler DriveSuite 100 Noblesville
